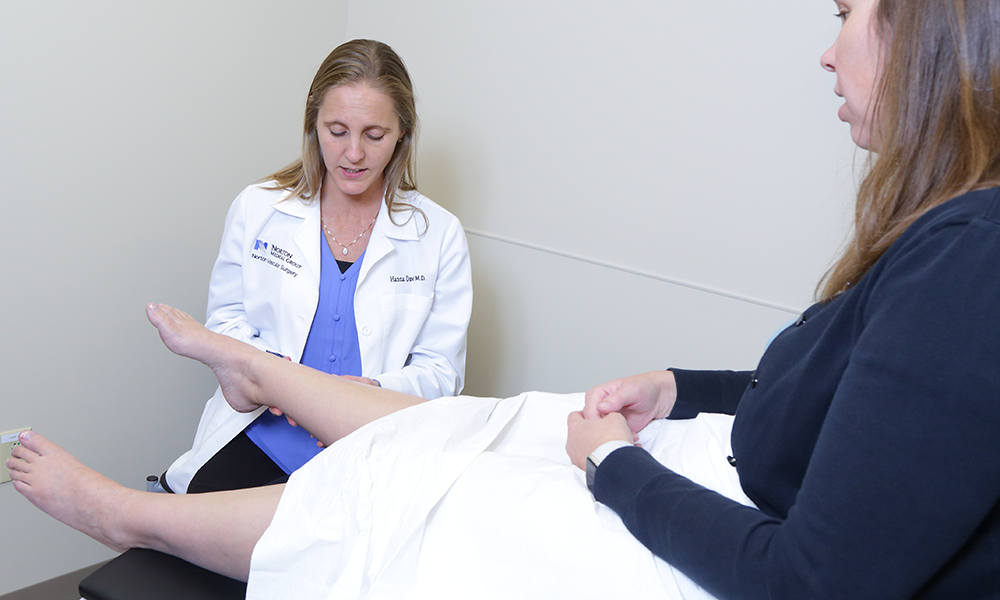
How to treat poor circulation in feet
If you have poor circulation in your feet, you’ve probably noticed weak or painful muscles when you walk, “pins and needles” tingling, pale skin, bulging veins or other symptoms.
Don’t take poor blood circulation lightly. Your primary care provider can determine whether simple treatment options like regular massages, compression socks, putting your feet up and eating better will remedy the condition.
Some cases of poor blood circulation can be a sign of peripheral artery disease, which if left untreated can damage your feet to the point of amputation and death.
Peripheral artery disease happens when plaque from high cholesterol builds up in arteries in your extremities, usually the legs or feet, making the blood vessel narrow and rigid. Blood clots can break from the plaque buildups causing complications. When this happens close to the heart or brain it can cause heart disease, heart attack and stroke.
Peripheral artery disease can advance to chronic limb-threatening ischemia (CLTI), where poor leg circulation has deteriorated to the point that your foot or part of your leg is at risk of needing amputation.
New treatment can help save limbs at risk of amputation
A new treatment, recently approved by the Food and Drug Administration (FDA), can restore blood flow and reduce risk of amputation for patients who have run out of other options, such as medication or surgery for CLTI. An estimated 1 in 5 patients with CLTI fit this description. CLTI affects up to 4 million Americans, resulting in more than 150,000 major amputations annually in the United States.
CLTI is the most serious form of peripheral artery disease and typically occurs in patients experiencing diabetes, coronary artery disease, obesity, high cholesterol and/or high blood pressure.
The primary surgical treatments to address CLTI symptoms are angioplasty or bypass surgery. In many patients, neither option is feasible because of extensive disease in the target arteries.
The treatment redirects blood flow around a blocked artery in the lower leg so blood can reach the feet. Norton Vascular Surgery, part of Norton Heart & Vascular Institute, is the first provider in Kentucky to offer the procedure.
“We’re thrilled to be able to offer our patients this first-of-its-kind procedure,” said Lauren M. Strait, M.D., vascular surgeon with Norton Heart & Vascular Institute. “It has the potential to greatly improve quality of life by reducing pain, enabling wound healing and, most important of all, preventing amputation.”
With the LimFlow System for transcatheter arterialization of deep veins, catheters are inserted from opposite directions — through a vein on the bottom of the foot, and an artery in the groin. Each is threaded through the blood vessels until they reach the area of the blood clot or other blockage.
At that point, the catheter in the artery pierces the vein, and the LimFlow device connects the two blood vessels. The vein carries oxygenated blood to the foot, then blood flow resumes its normal path back to the heart for recirculation.
Self-expanding stent grafts create a permanent conduit for blood flow from the artery into the vein.
The FDA approved LimFlow in September 2023 following a successful clinical trial.
In that study, published in the New England Journal of Medicine, 105 patients with CLTI underwent the LimFlow procedure. At six months, 76% avoided above-ankle amputation. Wounds were completely healed in 25% of patients and in the process of healing in 51%. No unexpected adverse events were reported.
Peripheral artery disease versus other vascular conditions
Peripheral artery disease and varicose veins are different conditions. Arteries carry oxygen-rich blood away from the heart out to the body, while veins return the depleted blood back to the lungs and heart for recirculation.
While peripheral artery disease is associated with blocked arteries, varicose veins typically are tied to leaking valves in the veins of the legs. Deep vein thrombosis is another condition affecting blood vessels, where clots form in veins far from the heart.
Because peripheral artery disease is caused by an underlying condition of cholesterol plaque buildup, or arteriosclerosis, treatment also means taking care of your risk for heart attack and stroke. If diagnosed early, peripheral artery disease can be managed by quitting smoking, managing diabetes and high blood pressure, lowering cholesterol and triglyceride levels in your blood, taking medication to prevent blood clots and exercising.
link




