Association between healthcare utilization patterns and long-term all-cause mortality after acute myocardial infarction discharge in South Korea
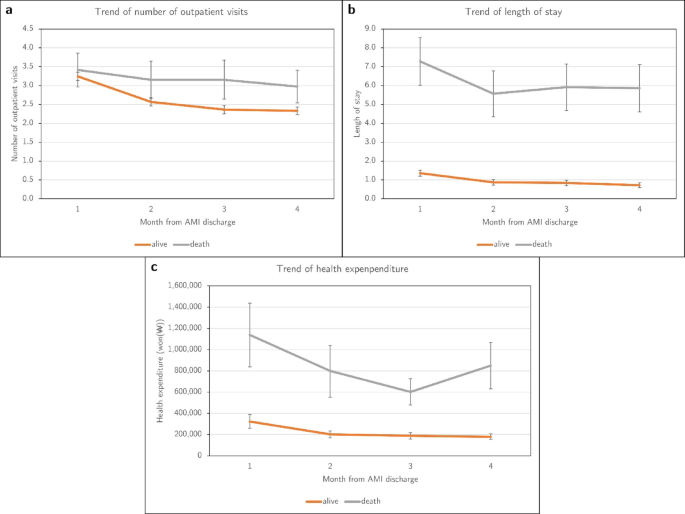
This study aimed to examine the healthcare utilization patterns of patients after surgery for AMI and predict their long-term mortality. The findings in the entire population revealed that the high-utilization (HR = 1.72; 95% CI, 1.10–2.70) and second-high-utilization (HR = 1.60; 95% CI, 1.06–2.42) groups had a higher risk of death after AMI surgery than the decreasing-utilization group. Among the elderly population, the high-utilization (HR = 1.96; 95% CI, 1.13–3.42) and second-high-utilization (HR = 2.05; 95% CI, 1.22–3.43) groups had a higher risk of death after AMI surgery than the decreasing-utilization group.
The high-utilization group and the second-high-utilization group exhibited similar disease patterns, but the average CCI score was higher in the high-utilization group. This could be considered one of the reasons for the differences in healthcare utilization. The Decreasing-utilization group and the Reverse J-shaped utilization group exhibit differences in the number of diagnosed diseases over time; decreasing utilization group had few diagnoses records in the fourth month and the reverse J-shaped utilization group had diagnostic records about common respiratory system disease, such as acute upper respiratory infections, bronchitis, emphysema and other chronic obstructive pulmonary diseases, and other diseases of upper respiratory tract and digestive system disease such as gastritis and duodenitis and other diseases of oesophagus, stomach and duodenum (Supplementary Tables 1 and 2).
In this study, we focused on healthcare utilization patterns to predict long-term mortality. It would be best if data could include clinical and laboratory test factors. However, the results of this study are valuable because obtaining healthcare utilization information is easier than obtaining clinical information. Healthcare utilization information is usually easily shared not only with patients but also with insurance companies and other health administrators. This information is useful for building health alert models.
In the case of AMI treatment, guidelines are well established.23,24,25,26 Although variations in health expenditure related to AMI due to external factors have been reported to be minimal,17 it could be considered that personal preference or physician-induced demand has little impact. In this study, we included not only healthcare utilization related AMI but also all types of healthcare utilization. Other healthcare utilization is important because it represents a latent variable reflecting the comorbidities of patients.
In this study, we found statistically significant differences in mortality in the elderly population because age is one of the main risk factors for cardiovascular diseases and frailty-related aging can be a health issue.27,28,29 Among individuals aged < 65 years, although no significant difference in mortality was observed, paying attention when developing future predictive models is necessary because the HR direction was similar. The HR direction observed in the second high-utilization and reverse J-shaped utilization groups was opposite because the number of deaths in the elderly population was much less than in that in individuals aged < 65 years. This result is similar to that reported in previous research.11.
Limitations and strengths
As the limitation of this study, healthcare utilization can be affected by institutional policies. Although the extent of impact of policies may vary because of differences in the point of view among the participants, in AMI treatment, it can be considered that the impact of policies is less because it is assured before the research period by insurance which is single system in Korea and where the Health Insurance Review and Assessment Service periodically conducts quality assessment of the healthcare benefits of AMI treatment in medical institutions.30.
There may be a concern regarding code mismatch for AMI. However, the code accuracy of this study could be considered to be higher because the code matching rate was approximately 91% in a previous study,31 and we included operation codes in this study. This study used the NHIS-NSC, which may have a small population. However, it can be considered sufficiently representative because the average number of individuals who underwent surgery for AMI in 1 year is approximately 21,993; the participants of this study accounted for approximately 2% of the total surgical population.32 NHIS-NSC is based on claim data, and a limitation is that clinical values are not reflected. However, we attempted to incorporate clinical aspects as much as possible by referencing AMI surgery guidelines and research, CCI, comorbidities, surgical treatment methods.23,33,34.
Unlike previous studies, this study focused on healthcare utilization and examined long-term mortality rates. Therefore, this study provides evidence that can be used for future personal health management and predictive research. The healthcare utilization information, such as outpatient visit days and LOS, which are easily collectible before tests or events occur in hospitals, could be used to predict mortality risks. These results could be beneficial for digital healthcare applications or public health surveillance. In the case of health expenditure, in Korea, a unified health expenditure is paid through a single health insurance system. However, it may be difficult to apply it because the method of paying health expenditure can vary depending on the characteristics of each country.
link



![South Korea Medical Devices Market Size, Share [2025-2032] South Korea Medical Devices Market Size, Share [2025-2032]](https://www.fortunebusinessinsights.com/accets/frontend/img/twitter-logo.png)


:quality(75)/https://asset.kgnewsroom.com/photo/pre/2026/01/23/63295e03-df22-48ba-9aa5-60a61921ed48_jpg.jpg)