Cardiovascular diseases (CVDs)

What are cardiovascular diseases?
Cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels. They include:
- coronary heart disease – a disease of the blood vessels supplying the heart muscle;
- cerebrovascular disease – a disease of the blood vessels supplying the brain;
- peripheral arterial disease – a disease of blood vessels supplying the arms and legs;
- rheumatic heart disease – damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria;
- congenital heart disease – birth defects that affect the normal development and functioning of the heart caused by malformations of the heart structure from birth; and
- deep vein thrombosis and pulmonary embolism – blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Heart attacks and strokes are usually acute events and are mainly caused by a blockage that prevents blood from flowing to the heart or brain. The most common reason for this is a build-up of fatty deposits on the inner walls of the blood vessels that
supply the heart or brain. Strokes can be caused by bleeding from a blood vessel in the brain or from blood clots.
What are the risk factors for cardiovascular disease?
The most important behavioural risk factors of heart disease and stroke are unhealthy diet, physical inactivity, tobacco use and harmful use of alcohol. The effects of behavioural risk factors may show up in individuals as raised blood pressure, raised
blood glucose, raised blood lipids, and overweight and obesity. These “intermediate risks factors” can be measured in primary care facilities and indicate an increased risk of heart attack, stroke, heart failure and other complications.
Cessation of tobacco use, reduction of salt in the diet, eating more fruit and vegetables, regular physical activity and avoiding harmful use of alcohol have been shown to reduce the risk of cardiovascular disease. Health policies that create conducive
environments for making healthy choices affordable and available are essential for motivating people to adopt and sustain healthy behaviours.
There are also a number of underlying determinants of CVDs. These are a reflection of the major forces driving social, economic and cultural change – globalization, urbanization and population ageing. Other determinants of CVDs include poverty,
stress and hereditary factors.
In addition, drug treatment of hypertension, diabetes and high blood lipids are necessary to reduce cardiovascular risk and prevent heart attacks and strokes among people with these conditions.
What are common symptoms of cardiovascular diseases?
Symptoms of heart attacks and strokes
Often, there are no symptoms of the underlying disease of the blood vessels. A heart attack or stroke may be the first sign of underlying disease. Symptoms of a heart attack include:
- pain or discomfort in the centre of the chest; and/or
- pain or discomfort in the arms, the left shoulder, elbows, jaw, or back.
In addition the person may experience difficulty in breathing or shortness of breath; nausea or vomiting; light-headedness or faintness; a cold sweat; and turning pale. Women are more likely than men to have shortness of breath, nausea, vomiting, and
back or jaw pain.
The most common symptom of a stroke is sudden weakness of the face, arm, or leg, most often on one side of the body. Other symptoms include sudden onset of:
- numbness of the face, arm, or leg, especially on one side of the body;
- confusion, difficulty speaking or understanding speech;
- difficulty seeing with one or both eyes;
- difficulty walking, dizziness and/or loss of balance or coordination;
- severe headache with no known cause; and/or
- fainting or unconsciousness.
People experiencing these symptoms should seek medical care immediately.
What is rheumatic heart disease?
Rheumatic heart disease is caused by damage to the heart valves and heart muscle from the inflammation and scarring caused by rheumatic fever. Rheumatic fever is caused by an abnormal response of the body to infection with streptococcal bacteria, which
usually begins as a sore throat or tonsillitis in children.
Rheumatic fever mostly affects children in developing countries, especially where poverty is widespread. Globally, about 2% of deaths from cardiovascular diseases are related to rheumatic heart disease.
Symptoms of rheumatic heart disease
Symptoms of rheumatic heart disease include: shortness of breath, fatigue, irregular heartbeats, chest pain and fainting.
Symptoms of rheumatic fever include: fever, pain and swelling of the joints, nausea, stomach cramps and vomiting.
Why are cardiovascular diseases a development issue in low- and middle-income countries?
At least three-quarters of the world’s deaths from CVDs occur in low- and middle-income countries. People living in low- and middle-income countries often do not have the benefit of primary health care programmes for early detection and treatment of people
with risk factors for CVDs. People in low- and middle-income countries who suffer from CVDs and other noncommunicable diseases have less access to effective and equitable health care services which respond to their needs. As a result, for many people
in these countries detection is often late in the course of the disease and people die at a younger age from CVDs and other noncommunicable diseases, often in their most productive years.
The poorest people in low- and middle-income countries are most affected. At the household level, evidence is emerging that CVDs and other noncommunicable diseases contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure.
At the macro-economic level, CVDs place a heavy burden on the economies of low- and middle-income countries.
How can the burden of cardiovascular diseases be reduced?
The key to cardiovascular disease reduction lies in the inclusion of cardiovascular disease management interventions in universal health coverage packages, although in a high number of countries health systems require significant investment and reorientation
to effectively manage CVDs.
Evidence from 18 countries has shown that hypertension programmes can be implemented efficiently and cost-effectively at the primary care level which will ultimately result in reduced coronary heart disease and stroke. Patients with cardiovascular disease
should have access to appropriate technology and medication. Basic medicines that should be available include:
- aspirin;
- beta-blockers;
- angiotensin-converting enzyme inhibitors; and
- statins.
An acute event such as a heart attack or stroke should be promptly managed.
Sometimes, surgical operations are required to treat CVDs. They include:
- coronary artery bypass;
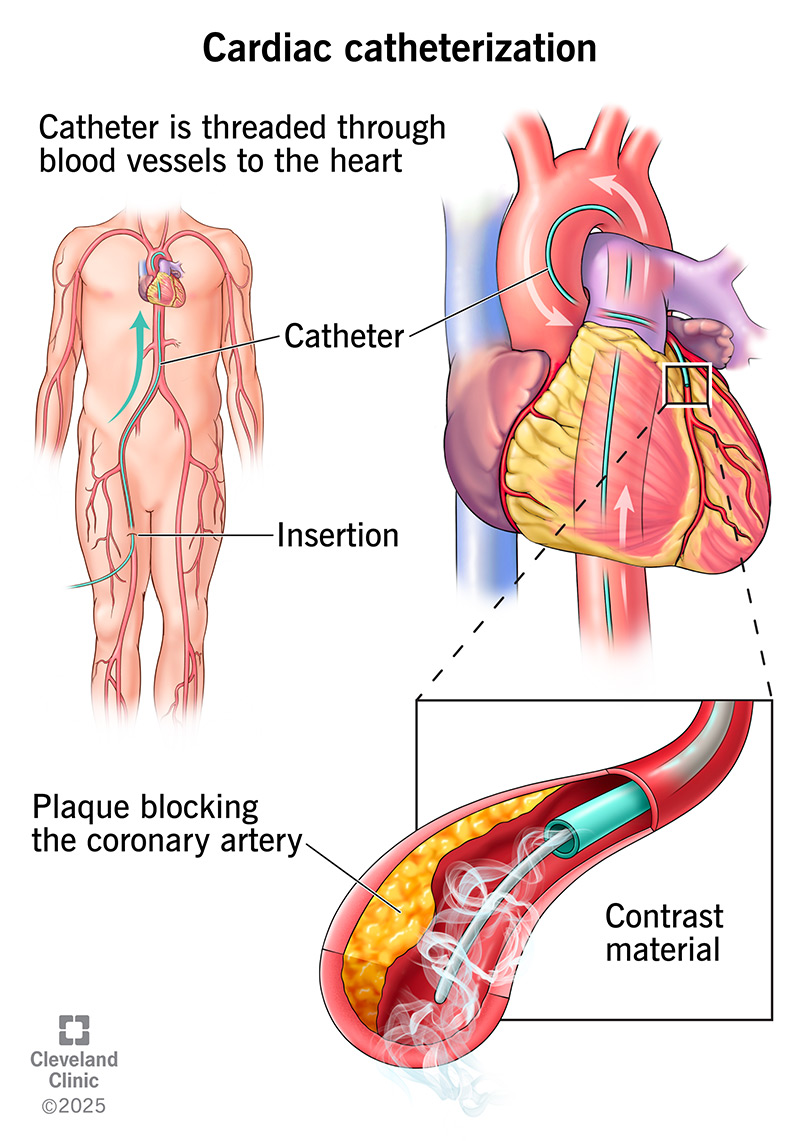
- balloon angioplasty (where a small balloon-like device is threaded through an artery to open the blockage);
- valve repair and replacement;
- heart transplantation; and
- artificial heart operations.
Medical devices are required to treat some CVDs. Such devices include pacemakers, prosthetic valves, and patches for closing holes in the heart.
WHO response
In 2013, WHO Member States agreed on global mechanisms to reduce the avoidable NCD burden including a “Global action plan for the prevention and control of NCDs 2013-2020”. This Plan aims to reduce the number of premature deaths from NCDs by 25% by 2025
through nine voluntary global targets. Two of the targets directly focus on preventing and controlling CVDs.
Target 6: Reduce global prevalence of raised blood pressure by 25% between 2010 and 2025.
Target 8: At least 50% of eligible people should receive drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes by 2025.
In addition, target 9 states that there should be 80% availability of the affordable basic technologies and essential medicines, including generics, required to treat major NCDs in both public and private facilities.
Achieving these targets will require significant investment in and strengthening of health systems.
WHO is currently working on increasing the normative guidance available for the management of acute coronary syndrome and stroke which will provide guidance in these important areas.
link